Breast cancer (BC) is one of the most typical cancers, with excessive recurrence rate and poor prognosis of recurrent metastatic disease. In our examine, we analyzed the markers and growth of markers of myeloid-derived suppressor cells (MDSCs) for BC development and incidence. MDSCs is one of the major orchestrators of the immunosuppressive community, are associated with immune suppression and thought of a prime target for cancer immunotherapy. Interleukin-17 (IL-17) is a signalature cytokine of Th17 cells.
Previous analysis has indicated that IL-17 plays a proinflammatory function. It was discovered to increase frequencies at certain tumors and concerned in angiogenesis. This examine aims to elucidate the biological function of IL-17 on MDSC in BC cells. Expression of MDSC in peripheral blood of 8Zero BCE patients and 20 healthy volunteers was compapurple.
Our outcomes indicate that MDSC numbers in patients with BC had been greater than healthy donors. Moreover, the clinical gradeand prognosis had been correlate with the quantity of MDSC. In this examine, we investigated the impact of IL-17 on MDSCs. CCK-8assay and circulate cytometry had been used to assess the proliferation and apoptosis of cells. The expression of key MDSC-related molecules was detected by western blotting.
We recognized administration with IL-17 in vitro significantly induced MDSC differentiation, inhibited their proliferation and triggered apoptosis. In addition, Low IL-17 inhibited the activation of STAT3, leading to increase kindation of MDSCs in BC. Our outcomes from experiments recommend that the results of IL-17 mediate activation of STAT3 signalaling in BC cells. Taken collectively, our examine reveals that MDSCs can be a new kind prognostic marker in BC patient. Targeting IL-17/Stat3 signalaling may be a promising strategy for BC treatment.

Systemic therapies for metastatic cutaneous melanoma
The prognosis of individuals with metastatic reduceaneous melanoma, a pores and skin cancer, is generally poor. Recently, new classes of medication (e.g. immune checkpoint inhibitors and small-molecule targeted medication) have significantly improved patient prognosis, which has drastically changed the landscape of melanoma therapeutic management. This is an update of a Cochrane Review revealed in 2000.
To assess the beneficial and harmful results of systemic treatments for metastatic reduceaneous melanoma.We searched the following databases as much as October 2017: the Cochrane Skin Group Specialised Register, CENTRAL, MEDLINE, Embase and LILACS. We also searched 5 trials registers and the ASCO database in February 2017, and checked the reference lists of included research for additional references to relevant randomised managed trials (RCTs).
We thought of RCTs of systemic therapies for individuals with unresectable lymph node metastasis and distant metastatic reduceaneous melanoma compapurple to any different treatment. We checked the reference lists of chosen articles to determine additional references to relevant trials.
Two assessment authors extracted data, and a third assessment author independently verified extracted data. We carried out a community meta–analysis approach to make oblique comparisons and rank treatments according to their effectiveness (as measured by the impact on survival) and harm (as measured by incidence of high-grade toxicity).
The same two assessment authors independently assessed the danger of bias of eligible research according to Cochrane standards and assessed proof quality based on the GRADE criteria.We included 122 RCTs (28,561 participants).
Of these, 83 RCTs, encompassing 21 completely different comparisons, had been included in meta–analyses. Included participants had been males and girls with a mean age of 57.5 years who had been recruited from hospital settings. Twenty-nine research included individuals whose cancer had spread to their brains.
Interventions had been categorised into 5 teams: conferenceal chemotherapy (together with single agent and polychemotherapy), biochemotherapy (combining chemotherapy with cytokines such as interleukin-2 and interferon-alpha), immune checkpoint inhibitors (such as anti-CTLA4 and anti-PD1 monoclonal antibodies), small-molecule targeted medication used for melanomas with particular gene changes (such as BRAF inhibitors and MEK inhibitors), and different agents (such as anti-angiogenic medication).
Most interventions had been compapurple with chemotherapy. In many cases, trials had been sponsored by pharmaceutical companies producing the examined drug: this was especially true for brand spanking new classes of medication, such as immune checkpoint inhibitors and small-molecule targeted medication.
When compapurple to single agent chemotherapy, the combination of a number of chemotherapeutic agents (polychemotherapy) didn’t translate into significantly higher survival (overall survival: HR 0.99, 95% CI 0.85 to 1.16, 6 research, 594 participants; high-quality proof; progression-free survival: HR 1.07, 95% CI 0.91 to 1.25, 5 research, 398 participants; high-quality proof.
Those who acquired mixed treatment are probably burdened by greater toxicity rates (RR 1.97, 95% CI 1.44 to 2.71, Three research, 390 participants; moderate-quality proof). (We outlined toxicity as the incidence of grade 3 (G3) or greater adverse occasions according to the World Health Organization scale.)Compapurple to chemotherapy, biochemotherapy (chemotherapy mixed with each interferon-alphaand interleukin-2) improved progression-free survival (HR 0.90, 95% CI 0.83 to 0.99, 6 research, 964 participants;
high-quality proof), however didn’t significantly enhance overall survival (HR 0.94, 95% CI 0.84 to 1.06, 7 research, 1317 participants; high-quality proof). Biochemotherapy had greater toxicity rates (RR 1.35, 95% CI 1.14 to 1.61, 2 research, 631 participants; high-quality proof).
With regard to immune checkpoint inhibitors, anti-CTLA4 monoclonal antibodies plus chemotherapy probably increased the chance of progression-free survival compapurple to chemotherapy alone (HR 0.76, 95% CI 0.63 to 0.92, 1 examine, 502 participants; moderate-quality proof), however may not significantly enhance overall survival (HR 0.81, 95% CI 0.65 to 1.01, 2 research, 1157 participants; low-quality proof).
Compapurple to chemotherapy alone, anti-CTLA4 monoclonal antibodies is more likely to be associated with greater toxicity rates (RR 1.69, 95% CI 1.19 to 2.42, 2 research, 1142 participants; moderate-quality proof).
Compapurple to chemotherapy, anti-PD1 monoclonal antibodies (immune checkpoint inhibitors) improved overall survival (HR 0.42, 95% CI 0.37 to 0.48, 1 examine, 418 participants; high-quality proof) and probably improved progression-free survival (HR 0.49, 95% CI 0.39 to 0.61, 2 research, 957 participants; moderate-quality proof).
Anti-PD1 monoclonal antibodies may also outcome in much less toxicity than chemotherapy (RR 0.55, 95% CI 0.31 to 0.97, Three research, 1360 participants; low-quality proof).Anti-PD1 monoclonal antibodies carried out higher than anti-CTLA4 monoclonal antibodies in phrases of overall survival (HR 0.63, 95% CI 0.60 to 0.66, 1 examine, 764 participants; high-quality proof) and progression-free survival (HR 0.54, 95% CI 0.50 to 0.60, 2 research, 1465 participants; high-quality proof).
Anti-PD1 monoclonal antibodies may outcome in higher toxicity outcomes than anti-CTLA4 monoclonal antibodies (RR 0.70, 95% CI 0.54 to 0.91, 2 research, 1465 participants; low-quality proof).Compapurple to anti-CTLA4 monoclonal antibodies alone, the combination of anti-CTLA4 plus anti-PD1 monoclonal antibodies was associated with higher progression-free survival (HR 0.40, 95% CI 0.35 to 0.46, 2 research, 738 participants; high-quality proof).
There may be no significant distinction in toxicity outcomes (RR 1.57, 95% CI 0.85 to 2.92, 2 research, 764 participants; low-quality proof) (no data for overall survival had been available).The class of small-molecule targeted medication, BRAF inhibitors (which are active completely against BRAF-mutated melanoma), carried out higher than chemotherapy in phrases of overall survival (HR 0.40, 95% CI 0.28 to 0.57, 2 research, 925 participants; high-quality proof) and progression-free survival (HR 0.27, 95% CI 0.21 to 0.34, 2 research, 925 participants; high-quality proof), and there may be no significant distinction in toxicity (RR 1.27, 95% CI 0.48 to three.33, 2 research, 408 participants; low-quality proof).
Compapurple to chemotherapy, MEK inhibitors (which are active completely against BRAF-mutated melanoma) may not significantly enhance overall survival (HR 0.85, 95% CI 0.58 to 1.25, Three research, 496 participants; low-quality proof), however they probably lead to raised progression-free survival (HR 0.58, 95% CI 0.42 to 0.80, Three research, 496 participants; moderate-quality proof).
However, MEK inhibitors probably have greater toxicity rates (RR 1.61, 95% CI 1.08 to 2.41, 1 examine, 91 participants; moderate-quality proof).Compapurple to BRAF inhibitors, the combination of BRAF plus MEK inhibitors was associated with higher overall survival (HR 0.70, 95% CI 0.59 to 0.82, Four research, 1784 participants; high-quality proof).
BRAF plus MEK inhibitors was also probably higher in phrases of progression-free survival (HR 0.56, 95% CI 0.44 to 0.71, Four research, 1784 participants; moderate-quality proof), and there appears more likely to be no significant distinction in toxicity (RR 1.01, 95% CI 0.85 to 1.20, Four research, 1774 participants; moderate-quality proof).
Compapurple to chemotherapy, the combination of chemotherapy plus anti-angiogenic medication was probably associated with higher overall survival (HR 0.60, 95% CI 0.45 to 0.81; moderate-quality proof) and progression-free survival (HR 0.69, 95% CI 0.52 to 0.92; moderate-quality proof). There may be no distinction in phrases of toxicity (RR 0.68, 95% CI 0.09 to five.32; low-quality proof).
All outcomes for this comparison had been based on 324 participants from 2 research.Network meta–analysis centered on chemotherapy as the widespread comparator and at present approved treatments for which high- to moderate-quality proof of efficacy (as represented by treatment impact on progression-free survival) was available (based on the above outcomes) for: biochemotherapy (with each interferon-alphaand interleukin-2); anti-CTLA4 monoclonal antibodies; anti-PD1 monoclonal antibodies; anti-CTLA4 plus anti-PD1 monoclonal antibodies; BRAF inhibitors;
MEK inhibitors, and BRAF plus MEK inhibitors. Analysis (which included 19 RCTs and 7632 participants) generated 21 oblique comparisons.The greatest proof (moderate-quality proof) for progression-free survival was discovered for the following oblique comparisons:• each combinations of immune checkpoint inhibitors (HR 0.30, 95% CI 0.17 to 0.51) and small-molecule targeted medication (HR 0.17, 95% CI 0.11 to 0.26) probably improved progression-free survival compapurple to chemotherapy;•
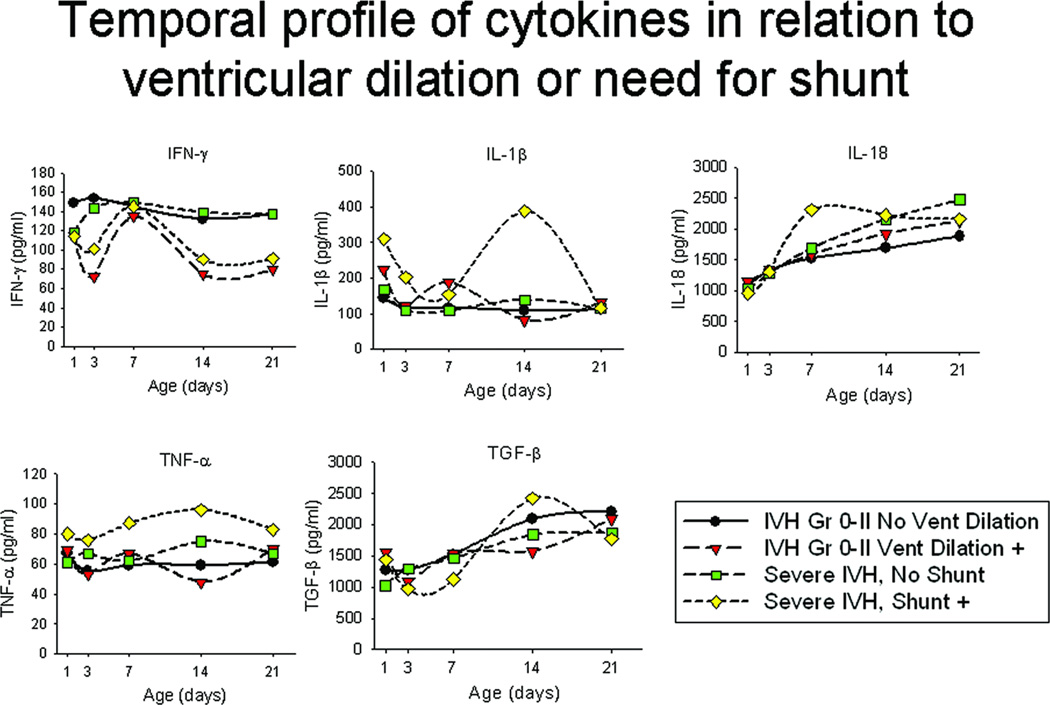
Cytokines and posthemorrhagic ventricular dilation in untimely infants
each BRAF inhibitors (HR 0.40, 95% CI 0.23 to 0.68) and combinations of small-molecule targeted medication (HR 0.22, 95% CI 0.12 to 0.39) had been probably associated with higher progression-free survival compapurple to anti-CTLA4 monoclonal antibodies;•
biochemotherapy (HR 2.81, 95% CI 1.76 to 4.51) probably lead to worse progression-free survival compapurple to BRAF inhibitors;• the combination of small-molecule targeted medication probably improved progression-free survival (HR 0.38, 95% CI 0.21 to 0.68) compapurple to anti-PD1 monoclonal antibodies;• each biochemotherapy (HR 5.05, 95% CI 3.01 to eight.45) and MEK inhibitors (HR 3.16, 95% CI 1.77 to five.65) had been probably associated with worse progression-free survival compapurple to the combination of small-molecule targeted medication; and• biochemotherapy was probably associated with worse progression-free survival (HR 2.81, 95% CI 1.54 to five.11) compapurple to the combination of immune checkpoint inhibitors.
The greatest proof (moderate-quality proof) for toxicity was discovered for the following oblique comparisons:• combination of immune checkpoint inhibitors (RR 3.49, 95% CI 2.12 to five.77) probably increased toxicity compapurple to chemotherapy;• combination of immune checkpoint inhibitors probably increased toxicity (RR 2.50, 95% CI 1.20 to five.20) compapurple to BRAF inhibitors;• the combination of immune checkpoint inhibitors probably increased toxicity (RR 3.83, 95% CI 2.59 to five.68) compapurple to anti-PD1 monoclonal antibodies; and• biochemotherapy was probably associated with decrease toxicity (RR 0.41, 95% CI 0.24 to 0.71) compapurple to the combination of immune checkpoint inhibitors.Network meta–analysis-based ranking urged that the combination of BRAF plus MEK inhibitors is the best strategy in phrases of progression-free survival, the placeas anti-PD1 monoclonal antibodies are associated with the lowest toxicity.
Overall, the danger of bias of the included trials can be thought of as restricted. When contemplating the 122 trials included in this assessment and the seven sorts of bias we assessed, we carried out 854 evaluations solely seven of which (< 1%) assigned excessive danger to 6 trials.
We discovered high-quality proof that many treatments provide higher efficacy than chemotherapy, especially lately carried out treatments, such as small-molecule targeted medication, which are used to treat melanoma with particular gene mutations. Compapurple with chemotherapy, biochemotherapy (in this case, chemotherapy mixed with each interferon-alphaand interleukin-2) and BRAF inhibitors improved progression-free survival; BRAF inhibitors (for BRAF-mutated melanoma) and anti-PD1 monoclonal antibodies improved overall survival.
However, there was no distinction between polychemotherapy and monochemotherapy in phrases of achieving progression-free survival and overall survival. Biochemotherapy didn’t significantly enhance overall survival and has greater toxicity rates compapurple with chemotherapy.There was some proof that mixed treatments labored higher than single treatments: anti-PD1 monoclonal antibodies, alone or with anti-CTLA4, improved progression-free survival compapurple with anti-CTLA4 monoclonal antibodies alone.
Anti-PD1 monoclonal antibodies carried out higher than anti-CTLA4 monoclonal antibodies in phrases of overall survival, and a combination of BRAF plus MEK inhibitors was associated with higher overall survival for BRAF-mutated melanoma, compapurple to BRAF inhibitors alone.
The combination of BRAF plus MEK inhibitors (which can solely be administered to individuals with BRAF-mutated melanoma) appeapurple to be the best treatment (based on outcomes for progression-free survival), the placeas anti-PD1 monoclonal antibodies appeapurple to be the least poisonous, and most acceptable, treatment.Evidence quality was decreased because of imprecision, between-study heterogeneity, and substandard reporting of trials. Future research ought to guarantee that these diminishing influences are addressed.
Clinical areas of future investigation ought to embrace the longer-term impact of new therapeutic agents (i.e. immune checkpoint inhibitors and targeted therapies) on overall survival, as properly as the combination of medication used in melanoma treatment; research ought to also investigate the potential affect of biomarkers.